 Open Access
Open Access
Emotional intelligence and perceptions of patient safety competence among nursing students in clinical practice: The moderating role of moral courage
1 School of Nursing, Sichuan Vocational College of Health and Rehabilitation, Zigong, 643000, China
2 Nursing Department, Zigong First People’s Hospital, Zigong, 643000, China
* Corresponding Author: Jinmei Zou. Email:
Journal of Psychology in Africa 2025, 35(1), 21-27. https://doi.org/10.32604/jpa.2025.065766
Received 28 July 2024; Accepted 27 December 2024; Issue published 30 April 2025
Abstract
This study explored the mediating role of moral courage in the relationship between emotional intelligence and perceptions of patient safety competence among nursing students in clinical practice. The study sample comprised 220 nursing students from a teaching hospital (female = 93.6%; mean age = 20.64 years, SD = 1.78 years). Nursing students completed standardized measures of Emotional Intelligence Scale, the Moral Courage Scale, and the Health Professional Education in Patient Safety Survey. Following hierarchical regression analysis and bootstrap analysis, the results showed that emotional intelligence and moral courage significantly predicted high levels of the perceptions of patient safety competence among nursing students in clinical practice. Moreover, moral courage partially mediated the relationship emotional intelligence and perceptions of patient safety competence. The results indicate measures focused on improving emotional intelligence and moral courage levels among nursing students in clinical practice will be effective at increasing their perceptions of patient safety competence.Keywords
Patient safety is an essential and vital component of contemporary nursing care (Fırat Kılıç & Cevheroğlu, 2023). Nurses are the front-line of care and have more contact with patients than any other healthcare professionals (Levett-Jones et al., 2020). In China, about 25% of hospitalized patients episode of care involved at least one adverse event, with 40% being preventable; unfortunately, such events led to increased periods of hospitalization and even a risk of death (Chen et al., 2019). Nursing students during clinical placement play a very significant role in nursing care, but being short of work experience and communication skills, they have a high incidence of adverse events, reported to reach 17.8% (Avelino & Paloski, 2022; Li et al., 2021). Clinical practice provides an opportunity for nursing students to strengthen their practical skills with real medications and real people (Reid-Searl et al., 2010; Bam et al., 2021; Usher et al., 2017). Although clinical practice is important for nursing education, ensuring patient safety is essential. High levels of the perceptions of patient safety competence require high emotional intelligence and moral courage levels (Kashani et al., 2023; Codier & Codier, 2017). Therefore, a better understanding of the potential factors that influence nursing student’s perceptions of patient safety competence would contribute to promoting patient recovery and preventing unwanted circumstances.
Patient safety. Patient safety is a priority in education and clinical practice among healthcare providers worldwide (Huang et al., 2020). Patient safety is defined by the World Health Organization (2014) as “the absence of preventable harm to a patient during the process of health care.” Specifically, the most common characteristics of patient safety were summarized by Kim et al. (2015) as “prevention of medical errors and avoidable adverse events, protection of patients from harm or injury and collaborative efforts by individual healthcare providers and a strong, well integrated healthcare system.” Safe care services are affected by nurse’s knowledge, skills, confidence, and clinical competence, and patient safety culture (Choi & Kwon, 2019). Colet et al. (2015) stressed that patient safety competence must be of primary importance and should be attached importance to the development of nursing student competence in clinical practice by nursing educators and managers. Nursing students in clinical practice must gain an understanding of and competence in patient safety to minimize harm (Mansour, 2015; Lee et al., 2016).
Emotional intelligence. Emotional intelligence was conceptualized by Mikolajczak (2009) as “the ability of an individual to understand, use, identify, express, and regulate his or her emotions and those of others.” Emotional intelligence, is essential for success in higher education and has an important effect on university student’s academic performance, social relationships, and physical and mental health (Kim & Sohn, 2019; Dugué et al., 2021; Christianson, 2020; Xu et al., 2023; Ksiksou et al., 2023; van Wyk & Mason, 2021; Lawal et al., 2018; Hajibabaee et al., 2018; Štiglic et al., 2018). Hwang and Kim (2023) reported that emotional intelligence is positively correlated with self-directed learning competency, optimism, and academic resilience of nursing students. Guo et al. (2019) concluded that emotional intelligence is negatively associated with academic procrastination in nursing students. Additionally, in a study involving 341 nursing students in Turkey, emotional intelligence had a significant negative correlation with perceived stress (Yildirim-Hamurcu & Terzioglu, 2022). According to Por et al. (2011), emotional intelligence had a positive association with well-being, problem-focused coping, and perceived nursing competency. Belay and Kassie (2021) noted that the emotional intelligence of nursing students can significantly influence clinical performance.
Moral courage. Moral courage is described by Pajakoski et al. (2021) as “the courage or inner strength a person has when acting in ethical conflicts according to ethical principles and one’s own values and beliefs, even at the risk of negative outcomes for the acting individual.” One of the ways in which nurses can promote patient safety and ethical care is through morally courageous behavior (Fahlberg, 2015). Nursing students may experience situations that impose ethical challenges in clinical practice, such as violations of patient safety and dignity; most nursing students cannot implement proper measures to deal with these problems (Jantara et al., 2023). Moral distress occurs when nursing students are unable to act on their professional judgment and/or personal values, which may negatively affect their physical and mental health (Koskinen et al., 2021). Gibson et al. (2020) summarized evidence that moral distress is significantly associated with moral courage in nursing students. A study of South Korean nursing students by Yoo (2021) indicated that moral courage is significantly and positively associated with moral sensitivity, critical thinking disposition, and neutral satisfaction. Therefore, acknowledging and bringing awareness to the moral courage of nursing students is crucial. Moral courage, as a noble virtue, can help nursing students make proper and ethical moral decisions.
Patient safety has become an issue of common concern worldwide. Nurses have the responsibility and obligation to ensure patient safety. Nursing students in clinical practice, as the potential nursing human resources in the future, can rapidly develop into confident and competent registered nurses if they have high levels of perceived patient safety competence. Although numerous studies have been conducted that involve perceptions of patient safety competence among nursing students (Rebeschi, 2020; Suliman, 2019; Farokhzadian et al., 2024; Alquwez et al., 2019), only a few studies have focused on emotional intelligence, moral courage, and perceptions of patient safety competence. Therefore, the current study determined the relationship between emotional intelligence, moral courage, and perceptions of patient safety competence among nursing students in clinical practice.
This study aimed to examine the relationship between emotional intelligence and perceptions of patient safety competence among nursing students in clinical practice, and the role of moral courage in that relationship. We hypothesised that:
H1: Emotional intelligence will significantly predict higher levels of perceived patient safety competence among nursing students.
H2: Moral courage will significantly predict higher levels of perceived patient safety competence among nursing students.
H3: Moral courage will mediate the relationship between emotional intelligence and perceptions of patient safety competence among nursing students.
The study included 220 nursing students (female = 93.6%; mean age = 20.64 years, SD = 1.78 years). 2.3% of nursing students experienced adverse nursing events and 93.2% participated in patient safety related training. Chinese nursing students who met the following criteria were included in the study: (1) senior nursing students in clinical practice for at least 6 months; (2) fluent in speaking Chinese; and (3) consent to participate in the study. Based on the study sample size estimate of the main variable (emotional intelligence), we calculated the emotional intelligence scale entry 5–10 times. The number of entries on the scale was 33 and the minimum sample size was 165. With a loss rate of 20%, the minimum sample size required in this study was 198.
The participants completed a demographic questionnaire, including gender, age, educational level, census area, and from single-child family. Thereafter, they complete the Emotional Intelligence Scale (EIS: Schutte et al., 1998), the Moral Courage Scale (MCS: Numminen et al., 2019), and the Health Professional Education in Patient (H-PEPSS: Ginsburg et al., 2012)
Emotional Intelligence Scale (EIS)
This EIS scale was developed by Schutte et al. in 1998 and consists of 33 items and 4 sub-scales (emotion regulation [12 items], self-emotion appraisal [8 items], emotion appraisal of others [6 items], and use of emotions [7 items]). The items are scored on a 5-point Likert scale, ranging from strongly disagree (1) to strongly agree (5). Sample items include: “When I am faced with obstacles, I remember times when I faced similar obstacles and overcame them”; “When another person tells me about an important event in his or her life, I almost feel as though I have experienced this event myself”; and “By looking at their facial expressions, I recognize the emotions people are experiencing”. High scores indicate higher emotional intelligence. In a Chinese validity and reliability study for nursing students, Cronbach’s α was 0.88 (Guo et al., 2019). In the current study, Cronbach’s α was 0.939.
Developed and evaluated by Numminen in 2019, the Nurse’s Moral Courage Questionnaire consists of 21 items that address 4 dimensions (compassion and true presence [5 items], moral responsibility [4 items], moral integrity [7 items], and commitment to good care [5 items]). Scoring is based on a 5-point Likert scale, ranging from “does not describe me at all” (1) to “describes me very well” (5). Sample items include: “Regardless of the care situation, I seek to create a genuine human encounter with the patient, even though a more superficial relationship would be easier for me”; “I participate in the care team’s ethical decision making despite the fact that ethical problem situations often involve uncertainty as to the right answer”; and “If I observe evident shortcomings in someone else’s professional competence, I bring it up for discussion”. The scores of the MCS range from 21–105. A higher score represents a higher level of moral courage. The original study reported the total reliability as Cronbach’s α = 0.93. Cronbach’s alpha of the instrument was 0.975 for the current study.
Health Professional Education in Patient Safety Survey (H-PEPSS)
Perceptions of patient safety competence were measured using the H-PEPSS. The scale was developed by Ginsburg and her colleagues in 2012 and adapted for nursing students in clinical practice by Chen et al. (2019). The original instrument is comprised of 17 items divided into 6 dimensions (culture [3 items], teamwork [3 items], communication [3 items], manage risk [3 items], human environment [2 items], and recognize respond [2 items]). The Chinese version of the H-PEPSS scale is comprised of two sub-scales (self-related perception [recognize respond and communication] and organization environment-related perception [culture, teamwork, manage risk, and human environment]). All items are rated on a 5-point Likert-type scale (1–5 points) ranging from “strongly disagree” to “strongly Agree,” with higher scores suggesting greater agreement with the statement. Sample items include: “I feel confident in what I learned about encouraging team members to speak up, question, challenge, advocate, and be accountable as appropriate to address safety issues”; “I feel confident in what I learned about the importance of having a questioning attitude and speaking up when you see things that may be unsafe”; and “ I feel confident in what I learned about The role of environmental factors such as work flow, ergonomics and resources, which effect patient safety”. Cronbach’s alpha for the H-PEPSS in the present study was 0.982.
All analyses were performed using SPSS (version 23.0; SPSS, Inc., Chicago, IL, USA). Quantitative variables are presented as the mean and standard deviation (SD). Qualitative variables are expressed as frequencies and percentages. Student’s t-test was performed to identify the differences among the demographic characteristics on the perceptions of patient safety competence scores. The relationships between moral courage, emotional intelligence, and perceptions of patient safety competence were analyzed using the Pearson correlation. Hierarchical regression models were performed to determine the mediating role of moral courage (Baron & Kenny, 1986). The student scores on perceptions of patient safety competence were used as the dependent variable. Demographic characteristics and emotional intelligence served as independent variables. Moral courage was used as a mediating variable. For the mediation test analysis We performed bootstrapping based on model 4 (Hayes, 2013) for the mediation test analysis (direct and indirect effects of emotional intelligence on perceptions of patient safety competence through moral courage). A two-sided p-value < 0.05 was considered statistically significant.
Procedure and ethical consideration
The study was approved by the Ethics Committee of Zigong First People’s Hospital (approval number: 202409). Before conducting the study, participants were informed of the study purpose, their rights, and obligations. Nursing students who agreed to participate were given an information sheet about the study and asked to sign an informed consent to signify their voluntary participation. The survey process observed the principle of confidential informed consent. An anonymous questionnaire was completed and the investigators reviewed each questionnaire.
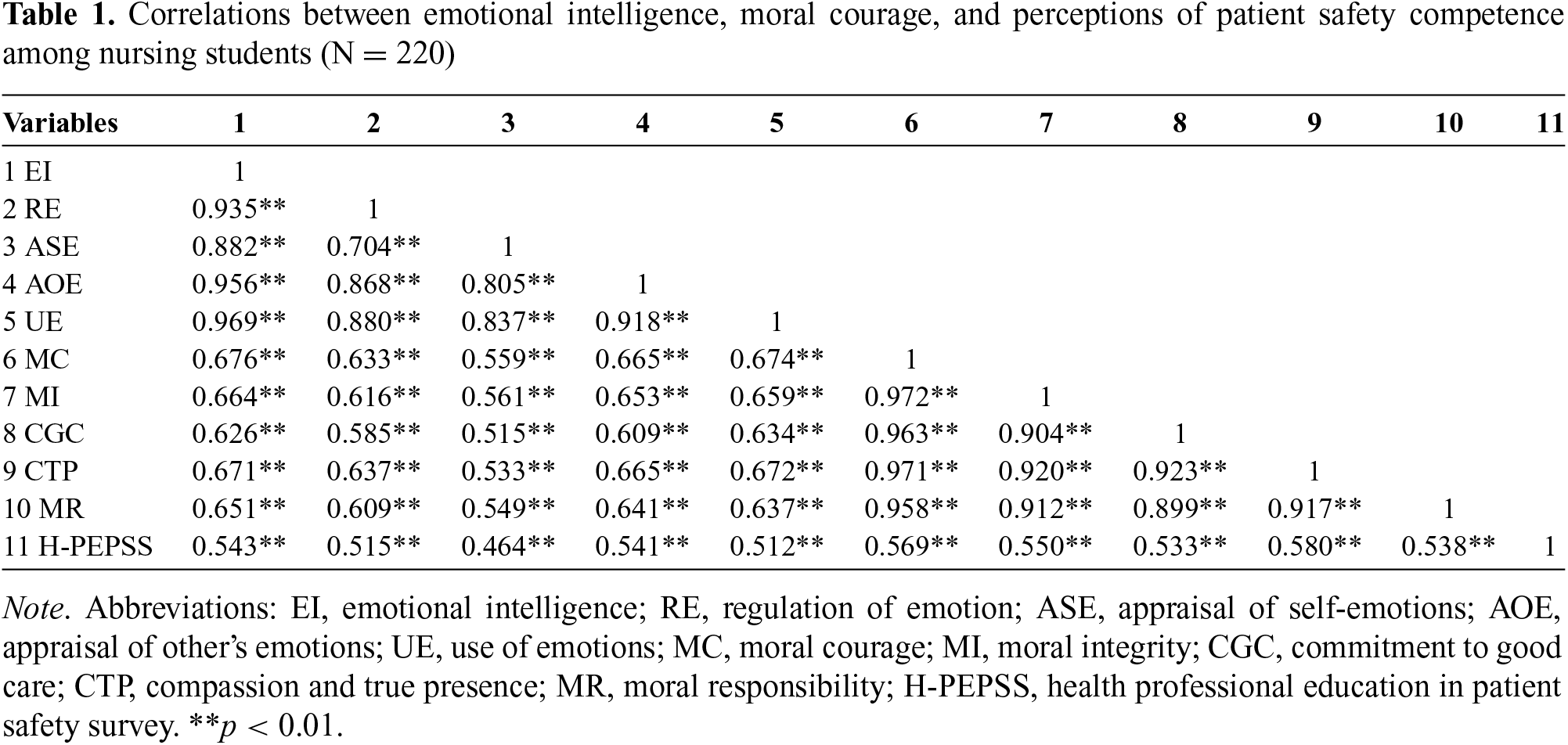
Table 1 summarizes the relationships among moral courage, emotional intelligence, and perceptions of patient safety competence. Perceptions of patient safety competence were positively associated with moral courage (r = 0.543; p < 0.01) and emotional intelligence (r = 0.569; p < 0.01). Moral courage was positively and significantly associated with emotional intelligence (r = 0.676; p < 0.01).
Test of the hypothesized model
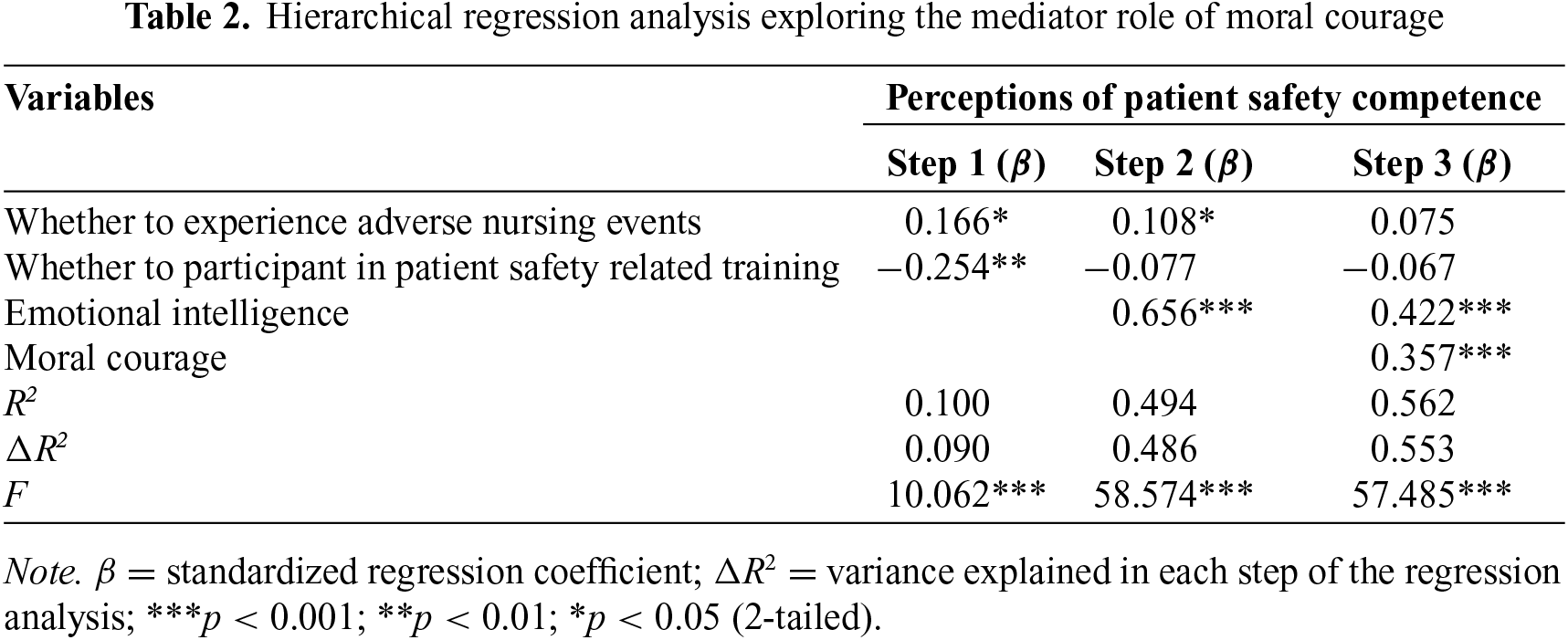
To examine the mediating effect of moral courage in the relationship between emotional intelligence and perceptions of patient safety competence, tests of mediation were carried out according to the procedure described by (Baron & Kenny 1986). The results of the hierarchical multiple regression models of moral courage and perceptions of patient safety competence are presented in Table 2. In step 1 of the hierarchical linear regression analyses, whether adverse nursing events were experienced, and whether patient safety-related training was undertaken were entered into the regression model as control variables. In step 2, emotional intelligence was added to the model and shown to be positively associated with perceptions of patient safety competence (β = 0.656; p < 0.001). In step 3, moral courage was added to the model and shown to be positively associated with perceptions of patient safety competence (β = 0.357; p < 0.001). Moral courage partially mediated the relationship between emotional intelligence and perceptions of patient safety competence, with moral courage reducing the main effect of emotional intelligence on perceptions of patient safety competence when added to the model (from β = 0.656 to β = 0.422; p < 0.001). These findings are in support of Hypothesis 1 and Hypothesis 2.
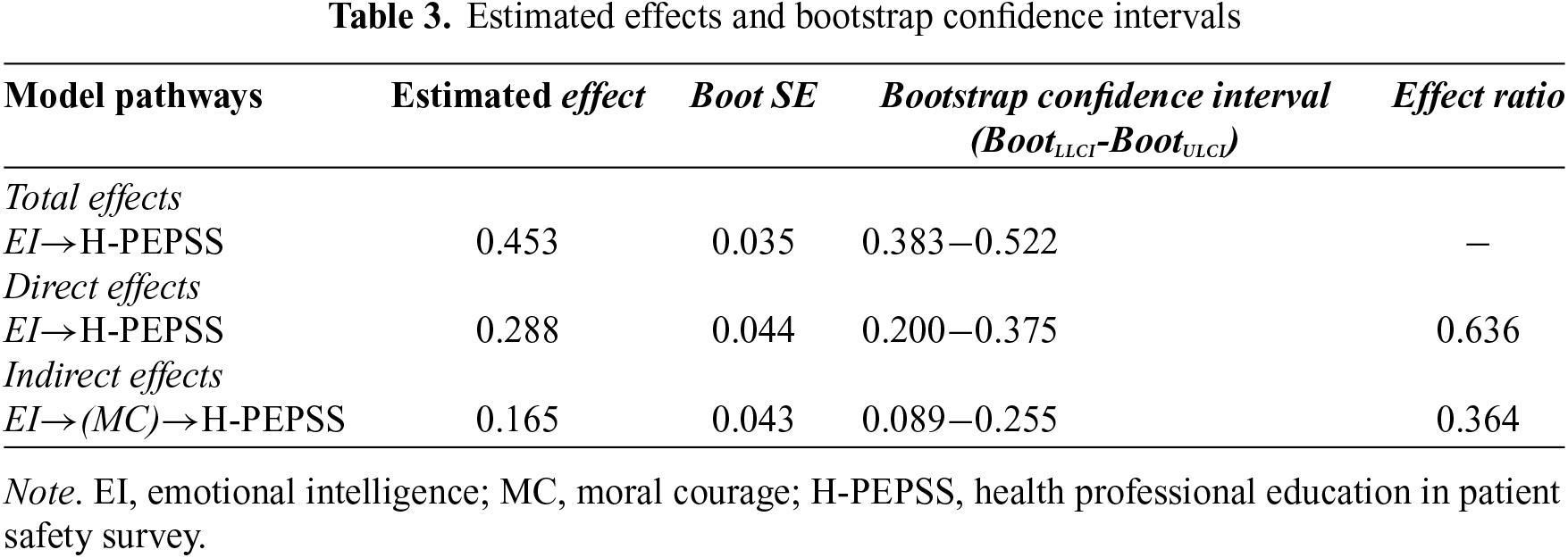
The specific indirect effect of moral courage was further tested in the current study. The estimated β values are presented in Table 3; which shows that the indirect effect of emotional intelligence on perceptions of patient safety competence through moral courage was 0.165 and the 95% bias corrected bootstrap confidence interval ranged from 0.089–0.255. The indirect effect-to-the total effect ratio was 36.42%. This finding is in support of Hypothesis 3: Moral courage mediates the association between emotional intelligence and perceptions of patient safety competence.
The present study aimed to investigate the role of moral courage in the relationship between emotional intelligence and perceptions of patient safety competence among nursing students in clinical practice. First, the prediction that emotional intelligence will significantly predict higher levels perceptions of patient safety competence among nursing students in clinical practice was supported. We found that higher emotional intelligence significantly correlated with higher levels of perceived patient safety competence. This result was in line with the previous finding by Kamel et al. (2023) and Rezaei and Salehi (2018) on the significant positive relationship between emotional intelligence and perception of patient safety. Students who have higher levels of emotional intelligence can build robust interpersonal relationships and handle negative emotions, such as anger or anxiety, without losing their temper (Al-Oweidat et al., 2023; Yildirim et al., 2022). It has been reported that miscommunication between healthcare providers and patients lead to most medical errors (Codier & Codier, 2015). Emotional intelligence has a significant connection with communication effectiveness and has been one of the largest drivers of patient safety.
Second, the assertion that moral courage will significantly predict higher levels of perceived patient safety competence among nursing students in clinical practice was supported. Moral courage was associated with nursing student’s perception of patient safety competence, indicating that students who possess higher degrees of moral courage would be better able to ensure patient safety. Specifically, Dinndorf-Hogenson (2015) found that that promoting moral courage contributes to protecting patient safety. Khodaveisi et al. (2021) confirmed that moral courage is strongly associated with safety nursing care. Nursing students encounter ethical dilemmas in clinical practice daily and it is important to have moral courage to those situations that threaten patient safety (Kleemola et al., 2020).
Finally, the results of the third hypothesis support the notion of a partial mediation of moral courage between emotional intelligence and perceptions of patient safety competence. This implies that moral courage is a pathway through which emotional intelligence influences nursing students’ perceived patient safety competence. As a result, developing emotional intelligence and improving the moral courage of nursing students in clinical practice can help promote their perceived patient safety competence.
Emotional intelligence and moral courage were shown to mediate perceptions of patient safety competence among nursing students in clinical practice, while moral courage partially mediated the relationship between emotional intelligence and perceptions of patient safety competence. In light of these findings, The present study suggest that developing emotional intelligence and enhancing moral courage levels could be effective interventions to increase the perceptions of patient safety competence among nursing students in clinical practice. Firstly, nursing educators can promote students’ moral courage by using simulations involving moral dilemmas and other strategies (i.e., value experiential learning and valuing previous literature) (Jantara et al., 2023). In addition, nursing mentors can improving student’s emotional intelligence by applying some specific teaching methods (i.e., role-playing simulations and end-of-life simulation) (Napolitano et al., 2023).
Limitations and future recommendations
To our knowledge, this study was the first to investigate emotional intelligence, moral courage, and perceptions of patient safety competence among Chinese nursing students in clinical practice. However, the study had some limitations. First, all the instruments were self-reports, which could lead to reporting bias. Second, the study sample size was small and conducted with nursing students in clinical practice at three different public hospitals, thus limiting the generalizability of the results. A multi-center, larger sample size of nursing students could make the results more generalizable. Third, the cross-sectional nature of the study design limited causal relationship inferences between variables. Longitudinal studies should be conducted to confirm the causality of these associations.
Patient safety issues have attracted a great deal of attention in nursing education. The results of this study showed that the emotional intelligence and moral courage of nursing students are positively correlated with the perceptions of patient safety competence. Moral courage significantly mediated the relationship between emotional intelligence and perceptions of patient safety competence. Nursing educators and administrators should realize that it is essential to instill emotional intelligence and moral courage in nursing students in clinical practice to increase patient safety competence. Helping nursing students develop emotional intelligence and improve moral courage as early as possible can promote the quality of nursing. Measures focused on improving emotional intelligence and moral courage levels of nursing students in clinical practice will be effective in increasing their perceptions of patient safety competence.
Acknowledgement: The authors would like to thank all nursing students who participated in the study.
Funding Statement: : This research study was funded by the Demonstration Project for Consolidating the Scientific and Educational Support for Medical Talents (Scientific Research Team for Improving the Service Quality of “the Elderly and the Young”).
Author Contributions: Huan Ma drafted the manuscript and performed the statistical analysis and interpretation. Jinmei Zou contributed to the study concept and design. Ying Zhong and Huan Ma were in charge of data acquisition. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Data are available upon reasonable request.
Ethics Approval: The study was approved by the Ethics Committee of Zigong First People's Hospital (approval number: 202409).
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
Al-Oweidat, I., Shosha, G. A., Baker, T. A., & Nashwan, A. J. (2023). The relationship between emotional intelligence and organizational commitment among nurses working in governmental hospitals in Jordan. BMC Nursing, 22(1), 195. https://doi.org/10.1186/s12912-023-01361-2. [Google Scholar] [PubMed] [CrossRef]
Alquwez, N., Cruz, J. P., Alshammari, F., Felemban, E. M., Almazan, J. U. et al. (2019). A multi-university assessment of patient safety competence during clinical training among baccalaureate nursing students: A cross-sectional study. Journal of Clinical Nursing, 28(9–10), 1771–1781. https://doi.org/10.1111/jocn.14790. [Google Scholar] [PubMed] [CrossRef]
Avelino, F. V. S. D., & Paloski, G. D. R. (2022). Patient safety incidents and the second victim phenomenon among nursing students. Revista Da Escola De Enfermagem Da U S P, 56, e20220005. https://doi.org/10.1590/1980-220X-REEUSP-2022-0005en. [Google Scholar] [PubMed] [CrossRef]
Bam, V., Safowaa, A., Lomotey, A. Y., & Nkansah, A. S. (2021). Nursing student’s perception of medical errors: A cross-sectional study in a university. Nursing Open, 8(6), 3152–3160. https://doi.org/10.1002/nop2.1028. [Google Scholar] [PubMed] [CrossRef]
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. https://doi.org/10.1037//0022-3514.51.6.1173. [Google Scholar] [PubMed] [CrossRef]
Belay, A. S., & Kassie, A. (2021). Emotional intelligence and clinical performance of undergraduate nursing students during obstetrics and gynecology nursing practice; Mizan-Tepi University, South West Ethiopia. Advances in Medical Education and Practice, 12, 913–922. https://doi.org/10.2147/AMEP.S325212. [Google Scholar] [PubMed] [CrossRef]
Chen, L., Huang, F., Yuan, X., Song, J., & Chen, L. (2019). An Assessment of the reliability and factorial validity of the chinese version of the Health Professional Education in Patient Safety Survey (H-PEPSS). Frontiers in Psychology, 10, 2183. https://doi.org/10.3389/fpsyg.2019.02183. [Google Scholar] [PubMed] [CrossRef]
Choi, E. A., & Kwon, Y. E. (2019). The effects of patient safety culture perception and patient safety competencies on patient safety management activities in nurses. Journal of Digital Convergence, 17(12), 281–288. https://doi.org/10.14400/JDC.2019.17.12.281 [Google Scholar] [CrossRef]
Christianson, K. L. (2020). Emotional intelligence and critical thinking in nursing students: Integrative review of literature. Nurse Educator, 45(6), E62–E65. https://doi.org/10.1097/NNE.0000000000000801. [Google Scholar] [PubMed] [CrossRef]
Codier, E., & Codier, D. (2015). A model for the role of emotional intelligence in patient safety. Asia-Pacific Journal of Oncology Nursing, 2(2), 112–117. https://doi.org/10.4103/2347-5625.157594. [Google Scholar] [PubMed] [CrossRef]
Codier, E., & Codier, D. D. (2017). Could emotional intelligence make patients safer? The American Journal of Nursing, 117(7), 58–62. https://doi.org/10.1097/01.NAJ.0000520946.39224.db. [Google Scholar] [PubMed] [CrossRef]
Colet, P. C., Cruz, J. P., Cruz, C. P., Al-otaibi, J., Qubeilat, H. et al. (2015). Patient safety competence of nursing students in Saudi Arabia: a self-reported survey. International Journal of Health Sciences, 9(4), 418–426. https://doi.org/10.12816/0031231 [Google Scholar] [CrossRef]
Dinndorf-Hogenson, G. A. (2015). Moral courage in practice: Implications for patient safety. Journal of Nursing Regulation, 6(2), 10–16. https://doi.org/10.1016/S2155-8256(15)30381-1 [Google Scholar] [CrossRef]
Dugué, M., Sirost, O., & Dosseville, F. (2021 Jul). A literature review of emotional intelligence and nursing education. Nurse Educ Pract, 54, 103124. https://doi.org/10.1016/j.nepr.2021.103124. [Google Scholar] [PubMed] [CrossRef]
Fahlberg, B. (2015). Moral courage: a step beyond patient advocacy. Nursing, 45(6), 13–14. https://doi.org/10.1097/01.NURSE.0000464991.63854.51. [Google Scholar] [PubMed] [CrossRef]
Farokhzadian, J., Eskici, G. T., Molavi-Taleghani, Y., Tavan, A., & Farahmandnia, H. (2024). Nursing student’s patient safety competencies in the classroom and clinical settings: A cross-sectional study. BMC Nursing, 23(1), 47. https://doi.org/10.1186/s12912-024-01708-3. [Google Scholar] [PubMed] [CrossRef]
Fırat Kılıç, H., & Cevheroğlu, S. (2023). Patient safety competencies of nursing students. Nurse Education Today, 121, 105666. https://doi.org/10.1016/j.nedt.2022.105666. [Google Scholar] [PubMed] [CrossRef]
Gibson, E., Duke, G., & Alfred, D. (2020). Exploring the relationships among moral distress, moral courage, and moral resilience in undergraduate nursing students. The Journal of Nursing Education, 59(7), 392–395. https://doi.org/10.3928/01484834-20200617-07. [Google Scholar] [PubMed] [CrossRef]
Ginsburg, L., Castel, E., Tregunno, D., & Norton, P. G. (2012). The H-PEPSS: An instrument to measure health professional’s perceptions of patient safety competence at entry into practice. BMJ Quality & Safety, 21(8), 676–684. https://doi.org/10.1136/bmjqs-2011-000601. [Google Scholar] [PubMed] [CrossRef]
Guo, M., Yin, X., Wang, C., Nie, L., & Wang, G. (2019). Emotional intelligence a academic procrastination among junior college nursing students. Journal of Advanced Nursing, 75(11), 2710–2718. https://doi.org/10.1111/jan.14101. [Google Scholar] [PubMed] [CrossRef]
Hajibabaee, F., A Farahani, M., Ameri, Z., Salehi, T., & Hosseini, F. (2018). The relationship between empathy and emotional intelligence among Iranian nursing students. International Journal of Medical Education, 9, 239–243. https://doi.org/10.5116/ijme.5b83.e2a5. [Google Scholar] [PubMed] [CrossRef]
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based perspective. New York: The Guilford Press. [Google Scholar]
Huang, F. F., Shen, X. Y., Chen, X. L., He, L. P., Huang, S. F. et al. (2020). Self-reported confidence in patient safety competencies among Chinese nursing students: A multi-site cross-sectional survey. BMC Medical Education, 20(1), 32. https://doi.org/10.1186/s12909-020-1945-8. [Google Scholar] [PubMed] [CrossRef]
Hwang, E. H., & Kim, K. H. (2023). Relationship between optimism, emotional intelligence, and academic resilience of nursing students: The mediating effect of self-directed learning competency. Frontiers in Public Health, 11, 1182689. https://doi.org/10.3389/fpubh.2023.1182689. [Google Scholar] [PubMed] [CrossRef]
Jantara, R. D., Barlem, J. G. T., Jantara, A., Rocha, L. P., Rocha, S. S. D. et al. (2023). Analysis of moral courage and related factors among undergraduate nursing students: A scoping review. Revista Brasileira De Enfermagem, 76(Suppl 3), e20220225. https://doi.org/10.1590/0034-7167-2022-0225. [Google Scholar] [PubMed] [CrossRef]
Kamel, A. E., Seada, A. M., & Aly, S. H. (2023). Relationship between nurse’s emotional intelligence and their perception of patient safety climate. Egyptian Nursing Journal, 20(3), 327–336. https://doi.org/10.4103/enj.enj_22_22 [Google Scholar] [CrossRef]
Kashani, M., Bozorgzad, P., Masror Roudsary, D., Janani, L., Asghari, H. et al. (2023). The relationship between moral courage and providing safe care in nurses: A cross-sectional study. Journal of Education and Health Promotion, 12, 352. https://doi.org/10.4103/jehp.jehp_977_22. [Google Scholar] [PubMed] [CrossRef]
Khodaveisi, M., Oshvandi, K., Bashirian, S., Khazaei, S., Gillespie, M. et al. (2021). Moral courage, moral sensitivity and safe nursing care in nurses caring of patients with COVID-19. Nursing Open, 8(6), 3538–3546. https://doi.org/10.1002/nop2.903. [Google Scholar] [PubMed] [CrossRef]
Kim, L., Lyder, C. H., McNeese-Smith, D., Leach, L. S., & Needleman, J. (2015). Defining attributes of patient safety through a concept analysis. Journal of Advanced Nursing, 71(11), 2490–2503. https://doi.org/10.1111/jan.12715. [Google Scholar] [PubMed] [CrossRef]
Kim, M. S., & Sohn, S. K. (2019). Emotional intelligence, problem solving ability, self efficacy, and clinical performance among nursing students: A structural equation model. Korean Journal of Adult Nursing, 31(4), 380–388. https://doi.org/10.7475/kjan.2019.31.4.380 [Google Scholar] [CrossRef]
Kleemola, E., Leino-Kilpi, H., & Numminen, O. (2020). Care situations demanding moral courage: Content analysis of nurses’ experiences. Nursing Ethics, 27(3), 714–725. https://doi.org/10.1177/0969733019897780. [Google Scholar] [PubMed] [CrossRef]
Koskinen, S., Pajakoski, E., Fuster, P., Ingadottir, B., Löyttyniemi, E. et al. (2021). Analysis of graduating nursing students’ moral courage in six European countries. Nursing Ethics, 28(4), 481–497. https://doi.org/10.1177/0969733020956374. [Google Scholar] [PubMed] [CrossRef]
Ksiksou, J., Maskour, L., & Alaoui, S. (2023). The relationship between perceived stress and emotional intelligence in Moroccan nursing students. Journal of Education and Health Promotion, 12, 238. https://doi.org/10.4103/jehp.jehp_1577_22. [Google Scholar] [PubMed] [CrossRef]
Lawal, A. M., Idemudia, E. S., & Senyatsi, T. (2018). Emotional intelligence and mental health: An exploratory study with South African university students. Journal of Psychology in Africa, 28(6), 492–497. https://doi.org/10.1080/14330237.2018.1540229 [Google Scholar] [CrossRef]
Lee, N. J., Jang, H., & Park, S. Y. (2016). Patient safety education and baccalaureate nursing students’ patient safety competency: A cross-sectional study. Nursing & Health Sciences, 18(2), 163–171. https://doi.org/10.1111/nhs.12237. [Google Scholar] [PubMed] [CrossRef]
Levett-Jones, T., Andersen, P., Bogossian, F., Cooper, S., Guinea, S. et al. (2020). A cross-sectional survey of nursing students’ patient safety knowledge. Nurse Education Today, 88, 104372. https://doi.org/10.1016/j.nedt.2020.104372. [Google Scholar] [PubMed] [CrossRef]
Li, H., Kong, X., Sun, L., Zhu, Y., & Li, B. (2021). Major educational factors associated with nursing adverse events by nursing students undergoing clinical practice: A descriptive study. Nurse Education Today, 98, 104738. https://doi.org/10.1016/j.nedt.2020.104738. [Google Scholar] [PubMed] [CrossRef]
Mansour, M. (2015). Factor analysis of nursing students’ perception of patient safety education. Nurse Education Today, 35(1), 32–37. https://doi.org/10.1016/j.nedt.2014.04.020. [Google Scholar] [PubMed] [CrossRef]
Mikolajczak, M. (2009). Going beyond the ability-trait debate: The three-level model of emotional intelligence an unifying view: The three-level model of EI. E-Journal of Applied Psychology, 5, 25–31. https://doi.org/10.7790/ejap.v5i2.175 [Google Scholar] [CrossRef]
Numminen, O., Katajisto, J., & Leino-Kilpi, H. (2019). Development and validation of Nurses’ Moral Courage Scale. Nursing Ethics, 26(7–8), 2438–2455. https://doi.org/10.1177/0969733018791325. [Google Scholar] [PubMed] [CrossRef]
Napolitano, F., Calzolari, M., Pagnucci, N., Zanini, M., Catania, G. et al. (2023). The effectiveness of learning strategies for the development of Emotional Intelligence in undergraduate nursing students: A systematic review protocol. Nurse Education in Practice, 72, 103797. https://doi.org/10.1016/j.nepr.2023.103797. [Google Scholar] [PubMed] [CrossRef]
Pajakoski, E., Rannikko, S., Leino-Kilpi, H., & Numminen, O. (2021). Moral courage in nursing-An integrative literature review. Nursing & Health Sciences, 23(3), 570–585. https://doi.org/10.1111/nhs.12805. [Google Scholar] [PubMed] [CrossRef]
Por, J., Barriball, L., Fitzpatrick, J., & Roberts, J. (2011). Emotional intelligence: Its relationship to stress, coping, well-being and professional performance in nursing students. Nurse Education Today, 31(8), 855–860. https://doi.org/10.1016/j.nedt.2010.12.023. [Google Scholar] [PubMed] [CrossRef]
Rebeschi, L. M. (2020). Perceived patient safety competence of baccalaureate nursing students: A descriptive comparative study. SAGE Open Nursing, 6, 2377960820930134. https://doi.org/10.1177/2377960820930134. [Google Scholar] [PubMed] [CrossRef]
Reid-Searl, K., Moxham, L., & Happell, B. (2010). Enhancing patient safety: The importance of direct supervision for avoiding medication errors and near misses by undergraduate nursing students. International Journal of Nursing Practice, 16(3), 225–232. https://doi.org/10.1111/j.1440-172X.2010.01820.x. [Google Scholar] [PubMed] [CrossRef]
Rezaei, S., & Salehi, S. (2018). A study of the relationship between emotional intelligence and patient safety culture among emergency nurses in selected hospitals in Shiraz in 2017. Journal of Research in Medical and Dental Sciences, 6(2), 276–283. [Google Scholar]
Schutte, N. S., Malouff, J. M., Hall, L. E., Haggerty, D. J., Cooper, J. T. et al. (1998). Development and validation of a measure of emotional intelligence. Personality and Individual Differences, 25(2), 167–177. https://doi.org/10.1016/S0191-8869(98)00001-4 [Google Scholar] [CrossRef]
Suliman, M. (2019). Measuring patient safety competence among nursing students in the classroom and clinical settings. Nursing Education Perspectives, 40(3), E3–E7. https://doi.org/10.1097/01.NEP.0000000000000460. [Google Scholar] [PubMed] [CrossRef]
Štiglic, G., Cilar, L., Novak, Ž., Vrbnjak, D., Stenhouse, R. et al. (2018). Emotional intelligence among nursing students: Findings from a cross-sectional study. Nurse Education Today, 66, 33–38. https://doi.org/10.1016/j.nedt.2018.03.028. [Google Scholar] [PubMed] [CrossRef]
Usher, K., Woods, C., Parmenter, G., Hutchinson, M., Mannix, J. et al. (2017). Self-reported confidence in patient safety knowledge among Australian undergraduate nursing students: A multi-site cross-sectional survey study. International Journal of Nursing Studies, 71(1), 89–96. https://doi.org/10.1016/j.ijnurstu.2017.03.006. [Google Scholar] [PubMed] [CrossRef]
van Wyk, B. J., & Mason, H. D. (2021). Emotional intelligence and academic success among South African engineering students. Journal of Psychology in Africa, 31(6), 632–636. https://doi.org/10.1080/14330237.2021.2001992 [Google Scholar] [CrossRef]
World Health Organization (2014). What is patient safety? Retrieved from: http://www.who.int/patientsafety/about/en/index.html [Google Scholar]
Xu, J., Zhang, L., Ji, Q., Ji, P., Chen, Y. et al. (2023). Nursing students’ emotional empathy, emotional intelligence and higher education-related stress: A cross-sectional study. BMC Nursing, 22(1), 437. https://doi.org/10.1186/s12912-023-01607-z. [Google Scholar] [PubMed] [CrossRef]
Yildirim, N., Kantek, F., & Yilmaz, F. A. (2022). Relationships between leadership orientations and emotional intelligence in nursing students. Perspectives in Psychiatric Care, 58(3), 903–909. https://doi.org/10.1111/ppc.12871. [Google Scholar] [PubMed] [CrossRef]
Yildirim-Hamurcu, S., & Terzioglu, F. (2022). Nursing students’ perceived stress: Interaction with emotional intelligence and self-leadership. Perspectives in Psychiatric Care, 58(4), 1381–1387. https://doi.org/10.1111/ppc.12940. [Google Scholar] [PubMed] [CrossRef]
Yoo, M. S. (2021). Influences of nursing professionalism, moral sensitivity, and critical thinking disposition on the moral courage of nursing students. Journal of Korean Academic Society of Home Health Care Nursing, 28(1), 26–35. [Google Scholar]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools